
2 Exercises for Plantar Fasciitis to Try at Home
Relieve foot pain from plantar fasciitis with these simple at home exercises.
If you’re struggling with throbbing or shooting pain in your heels, you’re not alone. Every year, close to one million Americans are diagnosed with plantar fasciitis — the most common source of heel pain.
Plantar fasciitis most often affects active adults between the ages of 40 and 70 — more frequently women than men. You’re more susceptible to plantar fasciitis if you’re a runner, if you’re pregnant, if you have flat feet, high arches or an uncommon foot position. Wearing high-heeled shoes or standing and jumping for long periods can also cause or aggravate the condition.
The largest ligament in your body is your plantar fascia, which lies directly beneath the skin on the bottom of the foot and connects your heel bone to your big toe to support the arch of your foot.
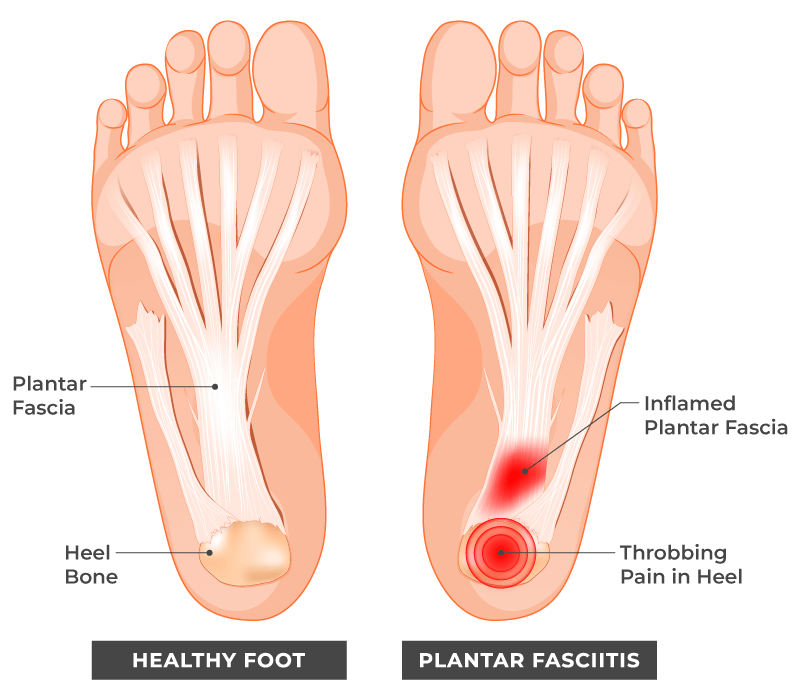
When this thick band of tissue becomes highly inflamed, you may feel anything from a dull throbbing or a stabbing pain in the sole or heel of your foot that can make walking or running difficult. This pain usually:
With time, the inflammation and foot pain may cause you to walk differently, and eventually this change in your gait can refer pain to your ankle, hip, back and even neck. Conversely, when misaligned, those body parts can trigger pain in your feet. That’s why remedies like cold packs and NSAIDs don’t provide long-term relief for referred pain (pain that originates in one place but is felt in another). Professional chiropractic care can.
Chiro One
Like a complicated pulley system, our muscles, tendons, ligaments, and bones never move independently — movement or tension in one part of the body always affects other parts. The inflammation in your plantar fascia could be a symptom of a full-body muscle tension pattern.
That means the pain you feel in the heels or soles of your feet may be directly triggered by other seemingly unrelated body parts like:
Your Ankles
When the muscle and fascia in your ankles lose flexibility, they limit your ankle’s range of motion. Gradually, this places more stress and weight on your plantar fascia, causing inflammation and tissue damage.
Your Calves
The fascia and muscle above your ankle weaves into your plantar fascia ligament. When your calf muscles (gastrocnemius) become too tight, your ankle can’t bend far enough. The strain this causes travels down your calf muscle tendons that attach to your heel bone, then into the tendons that attach your heel bone to your plantar fascia.
This tightness can contribute to both Achilles tendinopathies and plantar fasciitis pain. It makes sense that stretching the calves and feet routinely helps to reduce pain with plantar fasciitis.
Your Hips
When sedentary for too long, your lower back muscles (the quadratus lumborum and erector spinae) can pull your lumbar vertebrae closer together. This can tighten your hip flexors, which can tilt your pelvis forward, putting pressure on muscles and tendons in your thighs, knees, calves, and ankles all the way down to your plantar fascia.
Your Back
The pain and inflammation in your plantar fascia could be a symptom of a full-body muscle tension pattern. A compressed nerve in the back is connected to nerves in the buttocks, hips, thighs, knees, calves and finally, feet.
When researchers1 found that 74% of people with plantar heel pain had lower back pain, doctors began recommending treating the lower back to relieve referred pain in the feet.
If the tension builds up evenly across your lower back, you may feel pain in both feet equally. But if you have imbalanced tightness in the lower back muscles (iliopsoas and obliques) you’ll feel more pain in one foot than the other — and surprisingly, the tightness may be on the opposite side from the pain.
Your Pelvis
When your pelvis is tipped forward, or when one hip is hiked up higher than the other, they pull on your hamstrings, which:
The tension in your hamstrings pulls on the bones of your lower leg, trying to flex your knees by recruiting your lower leg muscles (gastrocnemius and plantaris).
These lower leg muscles attach to your Achilles tendon, which attaches to your heel bone. So, when these muscles are tight, they flex both your knee and your ankle.
When the ankle is plantar flexed, the muscles and connective tissues on bottom of the foot (plantar fascia) are tightened.
If you were lying down through all of this, you probably wouldn’t feel a thing. But if you spend a lot of time on your feet while your musculoskeletal pulley system is chronically tight and bearing the weight of your whole body, then plantar fascia pain is almost inevitable.
Healthcare providers in many specialties can perform an ultrasonography or magnetic resonance imaging to detect increased plantar fascia thickness and abnormal tissue. This doesn’t necessarily help determine the source of your referred pain and dysfunction.
Your Doctor of Chiropractic is trained to diagnose plantar fasciitis by performing an extensive physical exam to tract all the misalignments that may be contributing to your dysfunction. They also factor in your lifestyle issues and medical history to identify tender, inflamed areas that hold the root cause of your foot pain.
Cold therapy (icing) and over the counter NSAIDs can bring short term relief while you wait for your chiropractic adjustment, which will relieve pressure from your joints, including your plantar fascia ligament. Your DC may also perform the Graston technique — instrument-assisted soft tissue mobilization — to alleviate pain and inflammation in your feet.
These interventions will jump start the healing process, but it’s your prescribed active therapies that will ultimately complete it. Active therapies will also strengthen your surrounding muscles and improve your mobility.
Journal of Orthopedic Sports Medicine2 published a rigorous study demonstrating that when active therapies are prescribed in conjunction with myofascial release treatment patients required only 3 weeks of treatment! The patients who only received passive therapy took 21 weeks to recover.
During and after your recovery, your feet should always be properly supported. After all, they provide stability and functional balance, absorb shock and adjust to new terrains so you can stand, walk or run as much as you please.
Wearing custom orthotics (vs over the counter ones) is the best way to provide stability while reducing unnecessary stress and strain on your feet. Each Chiro One Custom Foot Orthotic is uniquely designed based on a 3D model of your feet, so they can’t slip, slide or press in the wrong place.
Check in with your nearest Chiro One doc at one of our welcoming open-plan clinics across the country. They’ll explore the root cause of your pain with a thorough exam, then personalize a care plan — a combination of gentle chiropractic adjustments and active therapies.
Subscribe and get news, articles & offers sent right to your inbox each month.
"*" indicates required fields
By subscribing you are agreeing to the Terms and Conditions and Privacy Policy.